What is the research gap?
Mental health comorbidities, defined as having two or more co-occurring mental health problems, present particular challenges, especially for UK military personnel. These comorbidities often make conditions more difficult to treat and are associated with greater adverse health outcomes, including reduced quality of life, difficulty in managing mental health symptoms and higher morbidity.
Currently, there is limited understanding of whether ex-serving Regular females experience different rates and patterns of mental health and hazardous alcohol use comorbidities compared to their male counterparts, and what factors might be associated with higher rates of these comorbidities. To address this gap in research, we analysed data from the King’s Centre for Military Health Research (KCMHR) Health and Wellbeing Cohort Study (Phase 4). We examined the rates and patterns of mental health and hazardous alcohol use comorbidities among UK Armed Forces ex-serving Regular personnel, with a particular focus on gender differences.
What did we find?
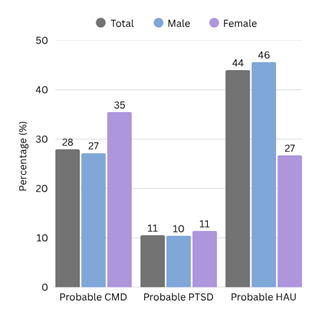
Our study of 2,294 ex-serving Regular UK military personnel (88% male, 12% female) showed that ex-serving females had significantly higher rates of common mental disorders (CMD) (35% compared to male 27%), but experienced comparable PTSD rates (10% for males vs 11% for females) (see Figure 1). Hazardous alcohol use (HAU) was significantly higher among ex-serving males compared to their female counterparts (46% vs 27%).
Figure 1: Mental health problem distribution overall and by gender.
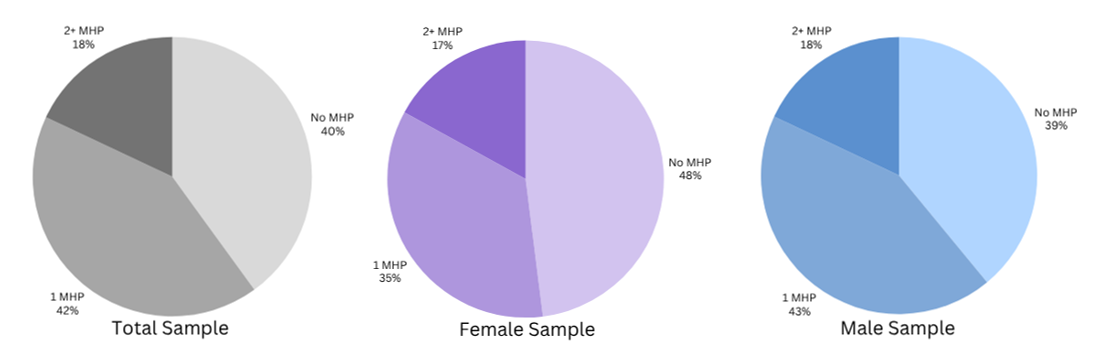
Subsequently, we looked at the number of mental health problems and hazardous alcohol misuse (MHPs) to see what percentage of the sample had 0, 1, or 2+ problems at the same time (see Figure 2). Of the total sample, 42% of ex-serving Regular personnel had one problem, while 18% reported comorbidities (≥2 problems). For ex-serving males, 43% had 1 problem, and 18% were comorbid. Ex-serving females in this study had slightly lower rates of comorbidities with 35% reporting 1 problem and 17% were comorbid.
Figure 2: Number of mental health problems and hazardous alcohol use (MHPs) overall and by gender.
We explored which of these conditions co-occurred together. We saw that CMD and HAU co-occurred most frequently within the whole comorbid sample (44%). We noted differences between male and female ex-serving Regular personnel as CMD and HAU were more commonly seen among males (45% of males, 34% of females), whereas CMD and PTSD were most frequently observed among female ex-serving personnel (42% of females, 26% of males). However, these differences were not significant, most likely due to small numbers.
Why is this important?
Our brief report indicates that mental health and hazardous alcohol use comorbidities are common among ex-serving Regulars and that patterns of co-occurring mental health problems differ in frequency by gender. This difference in pattern is mainly driven by higher rates of hazardous alcohol use among male ex-serving Regular personnel. It is recommended that healthcare professionals consider the co-occurence of mental health problems when ex-serving Regular personnel present to healthcare services in order to facilitate accurate diagnosis and to allow the targeting of appropriate treatment and support.
Authors: Sophie Lavarone, Dr Alex Smith, Dr Amber McKenzie, Dr Sharon Stevelink
Image: Cpl Danny Houghton